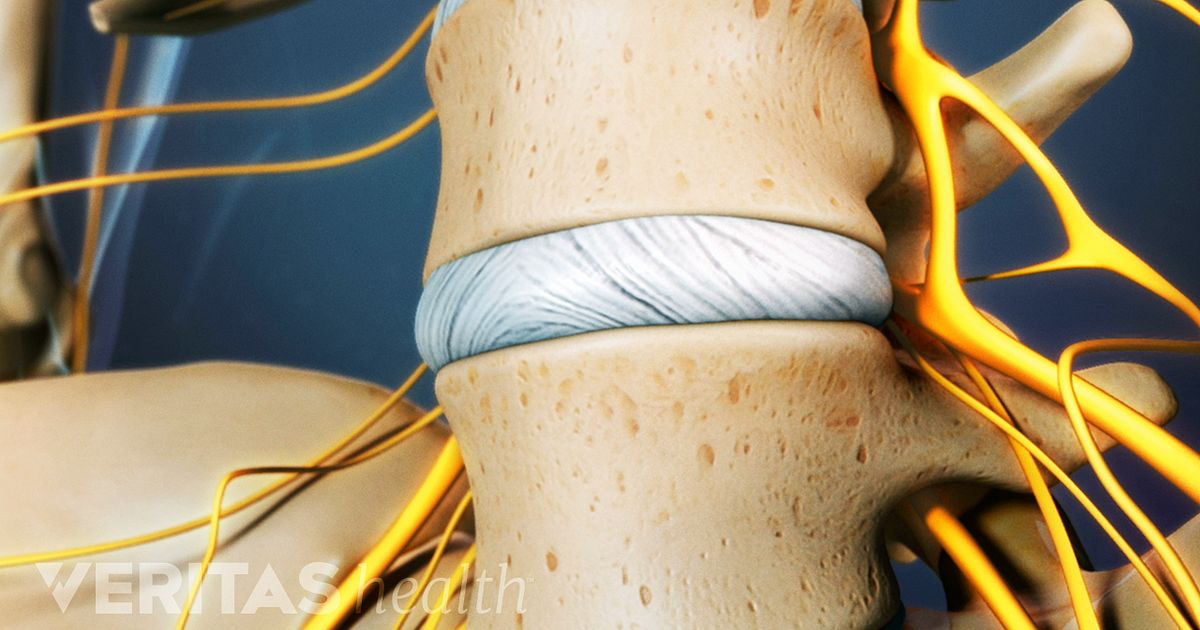
Lumbar provocative discography is an invasive diagnostic procedure for evaluation of diseases involving the intervertebral disc. It is performed in patients with persistent, severe low back pain. These patients have been found to have abnormal intervertebral spaces between vertebrae on magnetic resonance imaging (MRI).
It is currently used to determine whether the intervertebral disc is the source of back or neck pain. It is performed as a part of a presurgical evaluation. During discography, a contrast medium is injected into the disk and the patient’s response to the injection is noted; provocation of pain that is similar to the patient’s existing back or neck pain suggests that the disk might the source of the pain. Computed tomography (CT) is usually performed after discography to study anatomical changes in the disk and to identify possible sources of pain, such as clefts or tears.
Indications:
It is considered in patients with discogenic back pain when:
- planning of surgical intervention,
- prior conservative medical treatments, such as structured exercise, physical therapy, medications have failed
- imaging studies (CT, MRI) are inconclusive.
Procedure:
Preparation for the procedure includes having no food or drink after midnight. On the day of your exam, you will need to have a driver as you will not be permitted to drive home. You will receive iodinated x-ray dye, so you must inform the staff if you have iodine allergy. Premedication with steroids and Benadryl® is usually administered if that is the case. You will be asked to sign an informed consent form. The procedure is performed with the patient mildly sedated. Hence with the provocative portion of the exam. The actual procedure involves inserting a small bore needle into the disc levels with fluoroscopic guidance. Once in place, contrast is injected and images are acquired. Intradiscal anesthetic may be needed in some cases. Once the suspect area is identified, needles are inserted through the back into the intervertebral disc under fluoroscopic guidance. Fluid is then injected to pressurize the disc to elicit a pain response. This is repeated for various discs in random order. This is performed to assess the pain response and the suitability for recovery from possible discectomy. A CT scan of the area will be performed following the injection to identify leakage from the disc as a sign of spinal disc herniation. Recovery usually takes 2-3 hours.
Complications:
Like any interventional procedure, there is an increased risk of infection, which in this include acute epidural abscess, subdural empyema, prevertebral abscess, and discitis. Neural and spinal cord trauma and post-injection hematoma are other serious complications. Headaches can also occur.
What to expect after the procedure:
There is some discomfort during the procedure, for which a mild sedative or pain medication are given. The procedure is generally well tolerated. For regional soreness, ice packs may be applied as needed. Most patients are advised to take off work the next day.
